Transcatheter Aortic Valve Replacement: A New Gold Standard For Aortic Stenosis Management
What is Aortic Stenosis?
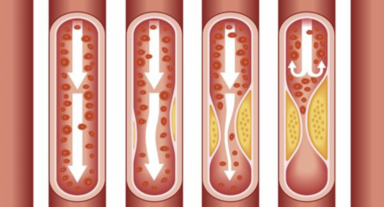
Aortic Stenosis is the medical term for narrowing of the aortic valve, within the heart. This is usually due to the valve deteriorating through years of use as people age but can also be due to abnormalities of the valve, present from birth.
How do you detect if I have Aortic Stenosis?
Aortic stenosis may be detected as patients develop symptoms of fatigue, shortness of breath, unexplained collapses or chest pain. This is due to a reduction in the blood and oxygen the heart is able to eject through the narrowed valve.
Alternatively, your healthcare provider may have detected a ‘murmur’ which is an additional heart sound and ordered further testing.
What investigations are required to confirm the diagnosis?
The principal way of confirming if a patient has aortic stenosis is through a transthoracic echocardiogram. This is a simple ultrasound of the heart which allows the cardiologist to visualise the valve and determine if it is failing to open normally.
Occasionally further testing can add additional information to help with the diagnosis and determine the best means of treatment. This can include exercise echocardiography to help detect the presence of symptoms when they are not clear, CT scanning to further assess the anatomy and determine the optimal form of treatment and invasive coronary angiography to detect any other cardiac issues which may need simultaneous treatment.
How is Aortic Stenosis Treated?
The traditional means of treating aortic stenosis was open heart surgery. This involves opening the breast bone, surgically removing the failed aortic valve and replacing it with a mechanical or tissue prosthetic (artificial) valve. This is an excellent treatment with very good clinical results in appropriately selected patients.
Since 2008 an alternate treatment has been available in Australia, Transcatheter Aortic Valve Replacement or TAVR. Through his involvement at Monash Health and Jessie McPherson Private Hospital, A/Prof Robert Gooley, leads the program, providing this treatment. This allows a new valve to be inserted through the artery in the groin and deployed within the existing narrowed valve. The original valve is displaced to the side and the new valve functions immediately. The delivery catheters are then withdrawn.
TAVR was initially used for patients who were deemed too high risk to undergo surgical aortic valve replacement but there is now evidence that many patients at low risk from surgery are also suitable for this treatment.
How do you determine the best treatment strategy?
All patients being considered for TAVR are managed by a collaborative team lead by A/Prof Rob Gooley. This team involves cardiologists, heart failure specialists, cardiothoracic surgeons and nurses. The team reviews all information before making a recommendation to the patient regarding their best form of treatment.
Where is treatment provided?
We are able to facilitate TAVR for suitable patients through Monash Health or Jessie McPherson Private Hospital.
What is the recovery following TAVR?
Patients are generally admitted the morning of their procedure. The procedure is performed under local anaesthesia and sedation in the cardiac catheterisation laboratory and takes about 90 minutes.
Following the procedure patients are transferred to the coronary care unit and are usually able to sit up after 6-12 hours. At this stage patients are able to walk gently. There may be some slight discomfort in the groin where the device was inserted but this is easily managed with mild pain relief.
The team see patients every day and together with the patient, family, nurses, physiotherapist and occupational therapist make an individual discharge plan. Patients are usually able to be discharged directly home after 2-4 days.
Patients normally notice an improvement in their breathing and fatigue levels within days and this can continue to improve for weeks and months depending on the level of deconditioning prior to the procedure.
What are the risks associated with TAVR and why may TAVR be the gold standard treatment?
While TAVR is less invasive than open heart surgery there are still risks associated with any procedure. A/Prof Gooley and the team discuss individual risks with each patient but large randomised studies comparing TAVR to surgery suggest that the overall risks are similar or reduced with TAVR in most patients.
This recent evidence that TAVR is as good or better than open surgery in many patients together with a reduced recovery time means it should be considered for all appropriate patients. Our cardiologists discuss whether it may be the optimal treatment strategy with all patients.
If I have aortic stenosis how can I be assessed?
Following referral from a general practitioner or other medical practitioner we arrange an initial review with a cardiologist to discuss the diagnosis and what further investigations may be required.
CATEGORIES: Heart Condition Management
TAGS: AORTIC STENOSIS, TRANSCATHETER AORTIC VALVE REPLACEMENT